Home Sleep Testing
The interpreting physician is making the assumption that you are sleeping; however, when done at home there is no way to know if you are sleeping or the depth of your sleep.
In detail…
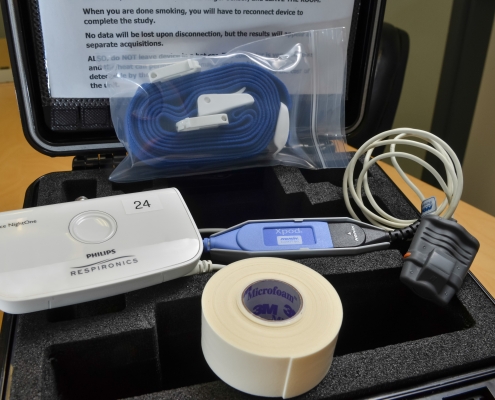
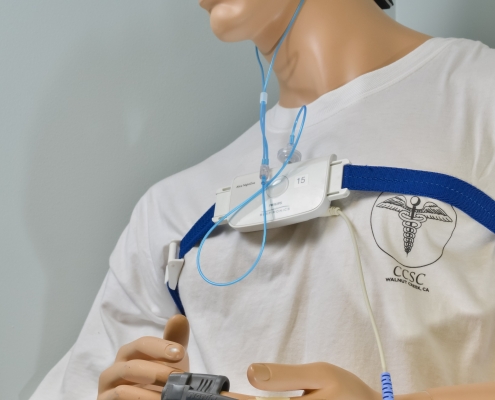
During a diagnostic sleep study, many types of data are recorded. When you come in for your appointment for the pickup of the equipment, a technician will explain how to use the device and you will then take it home. A small sensor will be applied near your nose and mouth to monitor airflow. Respiratory effort belts will be attached around your chest and abdomen. An Oximeter sensor will be taped onto one of your fingers to measure blood oxygen saturations levels. These monitoring devices are used to ensure an accurate evaluation of your sleep. Your movement will not be restrained; so, for example, if you need to go to the restroom or reach for a glass of water, you will be free to do so. You will wear the device for 1 night and then return the equipment to the facility.
Once the equipment is returned to the center your data will be compiled and downloaded. Later, a Sleep Technologist will review (hand-score) your study, page-by-page, and then send the results to an interpreting physician. The final report will be provided to your physician.
Results are generally ready 5-10 business days after your study is completed. You will want to make sure you set up a follow up appointment with your physician to go over your results.
Home sleep testing may be used as an alternative to polysomnography (PSG) for the diagnosis of OSA in patients with a high pretest probability of moderate to severe OSA. In some cases, health insurance companies will only authorize home sleep testing instead of attended studies, as it is less expensive.
Home sleep testing must be ordered or order must be reviewed by one of Contra Costa Sleep Center’s physicians after clinical evaluation of patient.
- Home testing is not appropriate for the diagnosis of OSA in patients with significant co-morbid conditions that may decrease the accuracy of the portable monitoring.
- Patients with co-morbid conditions such as pulmonary disease or heart disease.
- Patients suspected of having co-morbid sleep disorders.
- Low pretest probability of moderate to severe OSA.
- Patient not capable of complying with an unattended sleep study.
- Home testing is not appropriate for general screening of asymptomatic patients.
- Home testing may be indicated for the diagnosis of OSA in patients for whom in-laboratory PSG is not possible by virtue of immobility, safety, or critical illness.
- Home testing may also be indicated to monitor the response to non-CPAP treatments for OSA.
- A follow-up visit to review test results should be performed for all patients undergoing home sleep testing by referring physician. The report includes a recommendation for a Sleep Medicine consultation.
- Negative or technically inadequate home study tests in patients with a high pretest probability of moderate to severe OSA should prompt in-laboratory polysomnography.